Recurrent Pregnancy Loss
Recurrent Pregnancy Loss
Recurrent pregnancy loss (RPL) is generally defined as having had three or more consecutive pregnancy loses prior to 20 weeks’ gestation. RPL affects between 3% and 5% of couples. RPL becomes more prevalent with increasing female age, with an incidence of 10% to 15% in women in their twenties, rising to over 33% for women in their forties. In at least 50% of miscarriages, the fetus is chromosomally or genetically abnormal. Genetic abnormalities of the embryo may occur due to chance or occasionally secondary to chromosome aberrations in the parents. Other causes of RPL include abnormalities in the shape of the uterus. These uterine abnormalities may be due either to an abnormality present at birth or caused by benign tumors such as fibroids. Miscarriages may also occur as a result of intrauterine scarring caused by surgery and/or infections. In a small percentage of cases, antiphospholipid antibodies may be found in the maternal blood causing pregnancy loss.
Psychologic Impact
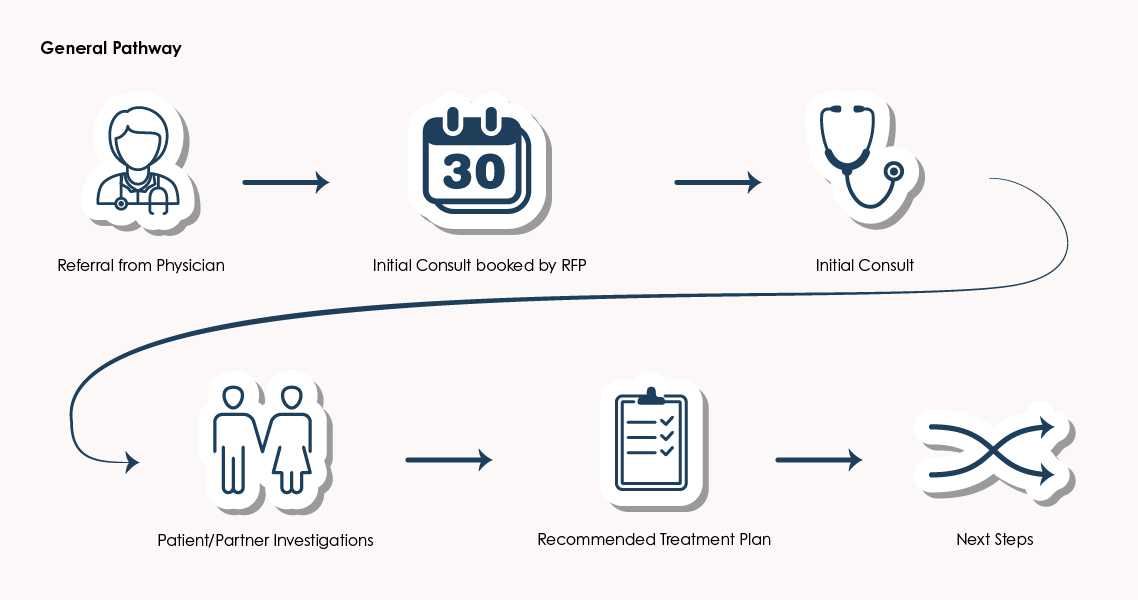
A miscarriage can cause significant psychologic grief for a couple and it is particularly difficult when a number of miscarriages happen. This may be made even worse if RPL is associated with infertility and increasing maternal age. It is common for couples to feel a sense of significant loss, emotional upset and helplessness after miscarriage. It can often be helpful for a couple in this situation to attend a self-help group or see a counselor. A referral will commonly be made to the RPL clinic after two or three consecutive losses.
Fertility Testing
The following tests may be ordered by your physician: A sonohysterogram (SHG) or hysterosalpingogram (HSG) may be performed to ensure the uterine cavity is normal. A genetic test or chromosomal test may be obtained from both partners to ensure there is no genetic abnormality, which is being passed on to the fetus that may cause RPL. This is a relatively uncommon cause of loss and is found in approximately 3% of couples. Tests may be performed for autoimmune disease and antiphospholipid antibodies. It is important to understand that in 50% of cases of RPL, no apparent cause will be found.
Treatment
If a uterine abnormality is found, it may generally be corrected by surgery. If a genetic problem is found in one parent a referral will be made to a specialist in genetic medicine for counselling. If autoimmune antibodies are found, blood thinners called heparin may be given during future pregnancies.
For more information on RPL, visit Resources